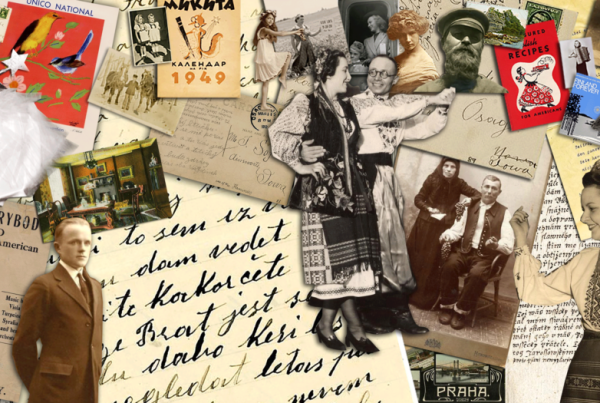
By Catherine Arnold

Teresa Bisson demonstrates virtual reality to her physical therapy class.
In video games, players in virtual reality (VR) goggles view their simulated actions as they stack blocks in Minecraft — or toss staplers and breakroom fruit in a workplace game called Job Simulator. It’s all in fun.
But in health care, patients experiencing “phantom limb” pain in nerve endings after an amputation can use such technology to virtually view the missing limb and exercise it, measurably easing their pain. Patients can learn to walk again after a stroke or knee surgery caused by an ACL tear — often at a faster pace while wearing goggles to picture their actions.
Such patient-based evidence shows VR can be a highly useful tool, says Teresa Bisson, Assistant Professor in the Division of Physical Therapy within the University of Minnesota Medical School. In particular, playing movement games in VR can help people who have experienced mobility difficulties following stroke, traumatic brain injury, or Parkinson’s disease.
Through a partnership with the University Libraries, Bisson has included VR in her classes where she has given her students a chance to experience the technology.
Getting started
While lecturing about the use of technology during her Neurorehabilitation course in 2015, Bisson realized it would best if students could actively try out and ask questions about technology. For several years, she had seen rehabilitation professionals explore VR and other technologies in their work, and she knew students would encounter technologies in the workplace.
“We’ve seen an explosion of ideas — from something as seemingly simple as an activity tracker or a cell phone app, to robotic treadmills and exoskeletons — that we might use to help people achieve rehabilitation goals and improve their quality of life.”
The following year during a tour with other physical therapy faculty of new VR systems in the Bio-Medical Library, Bisson met Jonathan Koffel, an emerging technology librarian who leads work around makerspaces, virtual reality, and other technologies. After discussing her idea with Koffel to use VR demos and other technologies in her classroom, they worked together with Del Reed, librarian for Allied Health Sciences, to make that happen.
Creative problem-solving
In classes, students try on and remove equipment to get a feel for it, discuss patients’ potential balance and nausea issues, think through steps like preventing trips on cords, and even talk about technical details like billing insurance for VR use.
Bisson hopes using technologies in class makes students feel familiar enough to get creative in choosing tools and methods for treatments. Longer term, she hopes knowing about VR can mean students are more likely to research and innovate further uses of the technologies.
“Virtual reality has the potential to provide more and improved treatments for patients in rehab, and by introducing our graduate students to that approach, they can be involved in leading that exploration,” explains Bisson.
Using game software for health
Software made expressly for rehabilitation is available, but Koffel says that using popular games (not made for health) can lower costs, increase accessibility, and allow therapists to personalize music, difficulty, mode (e.g., using one or both arms), and other factors to meet patient needs.
By demonstrating the game Beat Saber — in which users fight off flying blocks with light sabers — students can think about how commercial software can be creatively reused for therapy and rehab purposes.
Research¹ ² shows that patients are willing to do rehab for longer periods using VR than in real life, because they’re engaged in activities like painting, swinging a sword, or exploring a coral reef.
“This is one of the great things about VR,” says Koffel. “It makes the repetitive, but necessary, movements of rehabilitation more fun — and patients are more likely to do them.”
Thinking it through
Learning to apply critical thinking is part of each class too. After all, VR will not be available to patients in all cases. Limitations may include initial equipment expenses, a lack of support infrastructure or communication infrastructure for telerehabilitation in rural areas, and patient safety concerns.
“I wanted to guide my students toward being thoughtful users,” says Bisson, “so they ask questions and make informed decisions about incorporating technology in their physical therapy programs.”
Integrating technology into the learning process
Koffel and Reed are big parts of each class, guiding classroom experiences and discussions, and providing resources about the newest advances, products, and research literature related to the use of virtual reality in rehabilitation.
“I am very appreciative of the extensive support and resources available through the Libraries,” Bisson says. “Their expertise has helped me be more efficient in shaping course content and staying current with an ever-changing, evolving area of research and practice.”
“This technology is still new to many students; even those familiar with it are usually not thinking about clinical applications,” says Koffel. “By introducing them to these tools now, we can encourage them to think of innovative applications and help them become leaders in a new health care environment.”

Rendering of the new Health Sciences Library entryway.
We’re on the move!
In 2020, the Health Sciences Library be moving into the newly constructed Health Sciences Education Center, supporting innovative work like Teresa Bisson’s.
Learn more about our move and how you can support innovation in the health sciences as we provide technology rich environments and expertise that will promote new insights into teaching, learning, and research to address the health challenges of our time.
Give now